Case by Dr. Kristine Aadland.
Fig. 1. Preparation.
The patient’s old PFM bridge (shown here) was removed, and the existing preps for teeth #6 and #8 were modified with a medium chamfer with smooth and rounded edges to accommodate a 3-unit KATANA™ Zirconia bridge. There was no abutment for tooth #7, as that space serves as the pontic. Tooth #9 was similarly prepared to receive a single-unit KATANA™ crown.
Fig. 2. Define Restorations.
To begin, each restoration type is defined in the CEREC software, as the design mode (Biogeneric Individual), material type (KATANA™ Zirconia Block), and milling device (CEREC MC XL).
Fig. 3. Digital Impression.
A digital impression of the upper arch was performed using CEREC Primescan.
Fig. 4. Restoration Design.
The patient did not like the size of her centrals and wanted them smaller. She also didn’t like that her smile was slanted/canted. While designing, it really helps to use the patient’s old smile as a reference. This is why I used Bioindividual when designing the restorations, and added a BioCopy folder in the acquisition screen. I can ghost over the previous smile and readily see where I am.
Fig. 5. Restoration Design: Occlusal.
The BioCopy design function is also utilized to ensure a correct occlusal profile.
Fig. 6. Milling.
A KATANA™ Zirconia Block for bridge (14Z L) was used for the 3-unit bridge, and a KATANA™ Zirconia 12Z single-unit block was used for the single crown. The bridge block mills out in about 18 minutes, which is the fastest-milled chairside bridge block currently available.
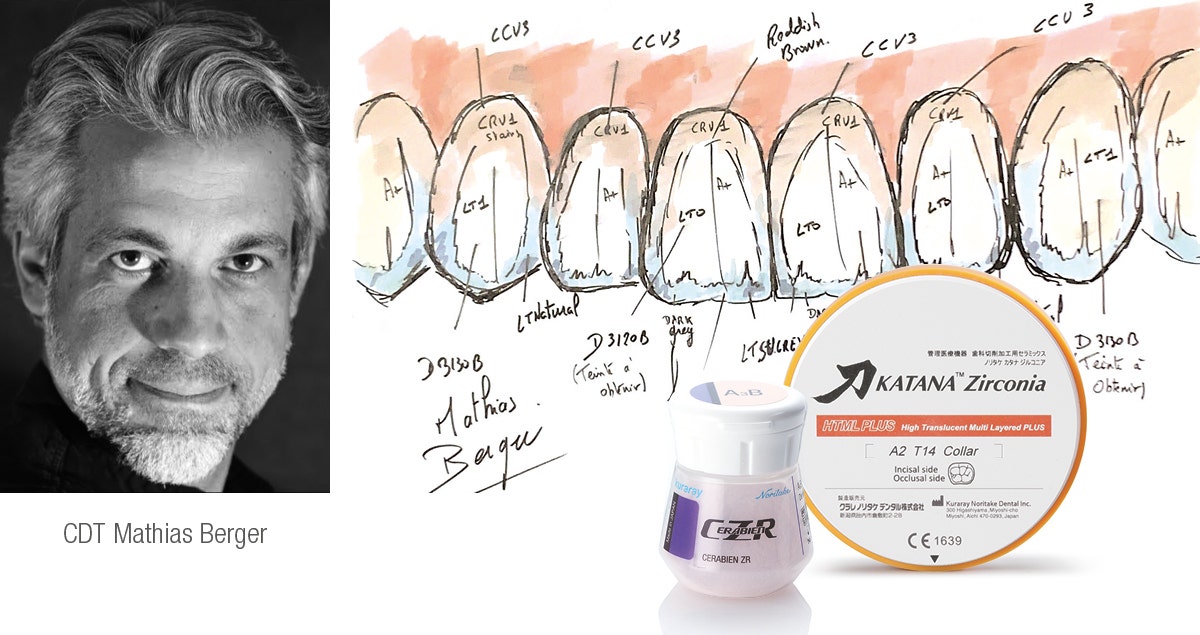
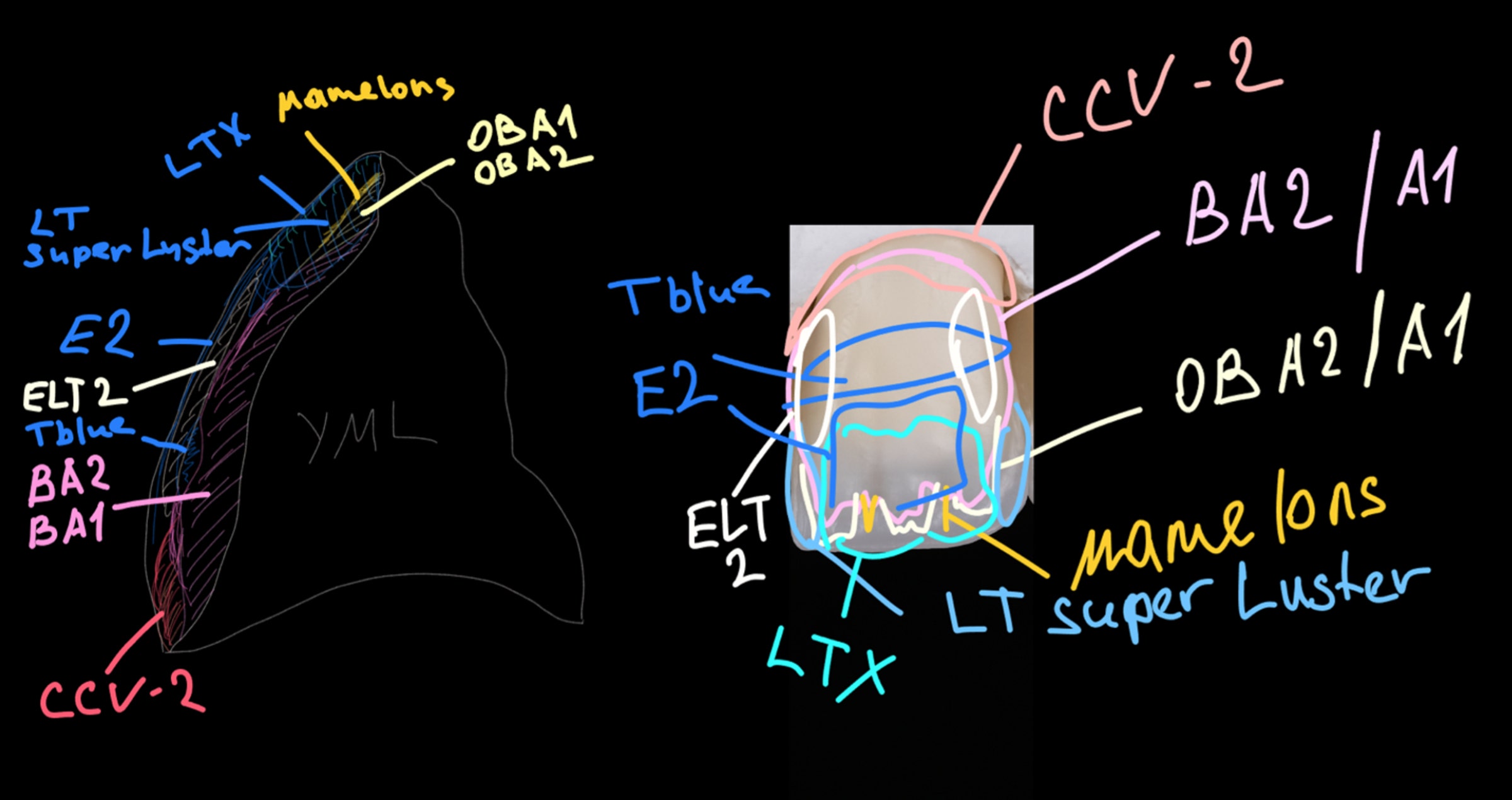
Fig. 7. Characterization & Sintering.
Kuraray Noritake CERABIEN™ ZR FC Paste Stain and Glaze Kit was used for characterizing. The colors are very natural and it is not simply a metal oxide like other stains, but actually adding porcelain, giving the restorations more vitality. The oven cycle is quick at approximately 10 minutes, which means multiple fires are easy to do without excess time.
Fig. 8. Seating & Final Smile.
PANAVIA™ SA Cement Universal and CLEARFIL™ Universal Bond Quick were used for cementation and bonding. I love the ease of use and clean-up with PANAVIA™ SA Cement Universal, and its MDP monomer creates a strong chemical bond to the tooth structure and zirconia. CLEARFIL™ Universal Bond Quick has a quick technique without reducing bond strengths, releases fluoride and has a low film thickness. I simply rub CLEARFIL™ Universal Bond Quick into the tooth for a few seconds and air dry. There is no need to light-cure, since it cures very well with PANAVIA™ SA Cement Universal. The patient was very happy with the results. She loved that she no longer saw metal margins, and her smile was much more uniform and lifelike.
DR. KRISTINE AADLAND