Time to celebrate PANAVIA’s 40th anniversary
Interview with Mitsunobu Kawashima
Manager, Technology Division of Kuraray Noritake Dental Inc.
In 1983 – exactly 40 years ago – PANAVIA™ EX was introduced in Japan as the first product of the PANAVIA™ family and the first product containing the original MDP monomer. Since then, the PANAVIA™ family of resin cements has been continuously expanded by developing new resin-cement materials that are precisely adjusted to the contemporary demands of dental practitioners. The current line-up of easy-to-use, high-performance adhesive luting materials is globally available and used by dental practitioners with high quality standards.
We had a conversation with Mr. Mitsunobu Kawashima about PANAVIA™ EX as a ground-breaking innovation in the field of dental resin cements and subsequent steps toward the current well-balanced resin cement portfolio. He is currently responsible for the development of chair-side materials in the Technology Division of Kuraray Noritake Dental Inc. (Kuraray Noritake Dental) and has been part of the team developing the many products of the PANAVIA™ family for more than 30 years.
The resin cements developed by the company before the introduction of PANAVIA™ EX contained the adhesive monomer Phenyl-P. Why did you decide not to use Phenyl-P in the new formulation?
At the time we decided to develop PANAVIA™ EX, we were engaged in the development of new adhesive monomers to replace Phenyl-P. The main aim of this project was an improvement of our products’ bond strength to metal alloys and dentin. Among the new adhesive monomers being developed, we decided to use the MDP monomer, because it features excellent bonding to tooth structure and metal alloys used in dentistry, as well as superb resistance to water. Incidentally, our first products to contain the original MDP monomer were the resin cement PANAVIA™ EX and the bonding agent CLEARFIL™ NEW BOND.
Where did the name PANAVIA™ come from?
The name “PANAVIA™” is a compound word consisting of “PAN” and “VIA”. The former is of Greek origin, and the latter is of Latin origin. “PAN” means “everything” and “VIA” means “way” or “method”. Consequently, the name “PANAVIA” describes a “method for bonding everything”; it represents our desire to have products launched under the umbrella of the PANAVIA™ brand recognized as dental materials that can bond to all types of restoration and tooth structure.
Would you please tell us the story behind the development of PANAVIA™ EX?
Back in the early 1980s, it was indispensable for us to develop new adhesive monomers as a part of our project to develop a new resin cement with unprecedented adhesive properties. In this context, we conducted a comprehensive literature search for compounds thought to be involved in adhesion. At the same time, we carried out a variety of R&D activities, including basic research to quantitatively clarify the relationship between the molecular structures of monomers and their adhesive qualities, synthesis trials of various monomers and bond strength tests. Consequently, we succeeded in developing the MDP monomer that had the physical properties we were working to obtain. Following the development of that MDP adhesive monomer, we were finally able to create PANAVIA™ EX in our laboratory. In early 1982, we completed the first prototype of PANAVIA™ EX for external evaluation and asked a dental college in Japan to evaluate it. He found that the prototype cement might cure too quickly in clinical use. This was due to the fact that we had not taken into account the difference between room temperature and intraoral temperature, which has a huge impact on the curing time. This error led us to recognize how important clinical evaluations are during the development of dental materials. To this day, we continue to place great importance on the opinions of clinicians whenever a new material is being developed.
The name “PANAVIA™” is a compound word consisting of “PAN” and “VIA”. The former is of Greek origin, and the latter is of Latin origin. “PAN” means “everything” and “VIA” means “way” or “method”.
What were the key technological features of this new PANAVIA™ EX cementation system?
The system had five key features: Appropriate film thickness, appropriate flow properties of the paste, radiopacity, improved bond strength and improved surface-cure characteristics. At the time that PANAVIA™ EX was developed, a film thickness of 30 μm or less was desired for luting cements. The largest components we wanted to use in the formulation – the silica filler particles present in our composite resin – had a maximum particle diameter of 50 μm. We were able to achieve a film thickness of 30 μm or less by significantly extending the silica grinding time, which made the filler particles much finer. An appropriate paste consistency – a low level of viscosity and good flowability – was achieved by using low-viscosity monomers for PANAVIA™ EX. In order to make the cement radiopaque, we dispersed radiopaque filler within the powder component. In fact, we were convinced that it was essential to be able to check for the presence of excess cement under the gingival margins after a restoration was placed. The increase in bond strength was achieved by blending the MDP monomer into the liquid component.
What about the surface-cure characteristics of the cement?
Every dental practitioner knows that the surface of resin cements must be protected from oxygen in the air in order to cure properly. For this purpose, we developed OXYGUARD, a water-soluble gel material. It is applied to the restoration margins to cover the unpolymerized resin cement surface and protect it from exposure to oxygen. In this way, the formation of an oxygen inhibition layer – a layer of uncured resin on the surface that compromises the marginal integrity of the restoration – is prevented and an intact, fully polymerized cement surface can develop. In this way, the use of OXYGUARD has contributed greatly to improving the cure characteristics of cements.
What do today’s PANAVIA™ products and PANAVIA™ EX have in common?
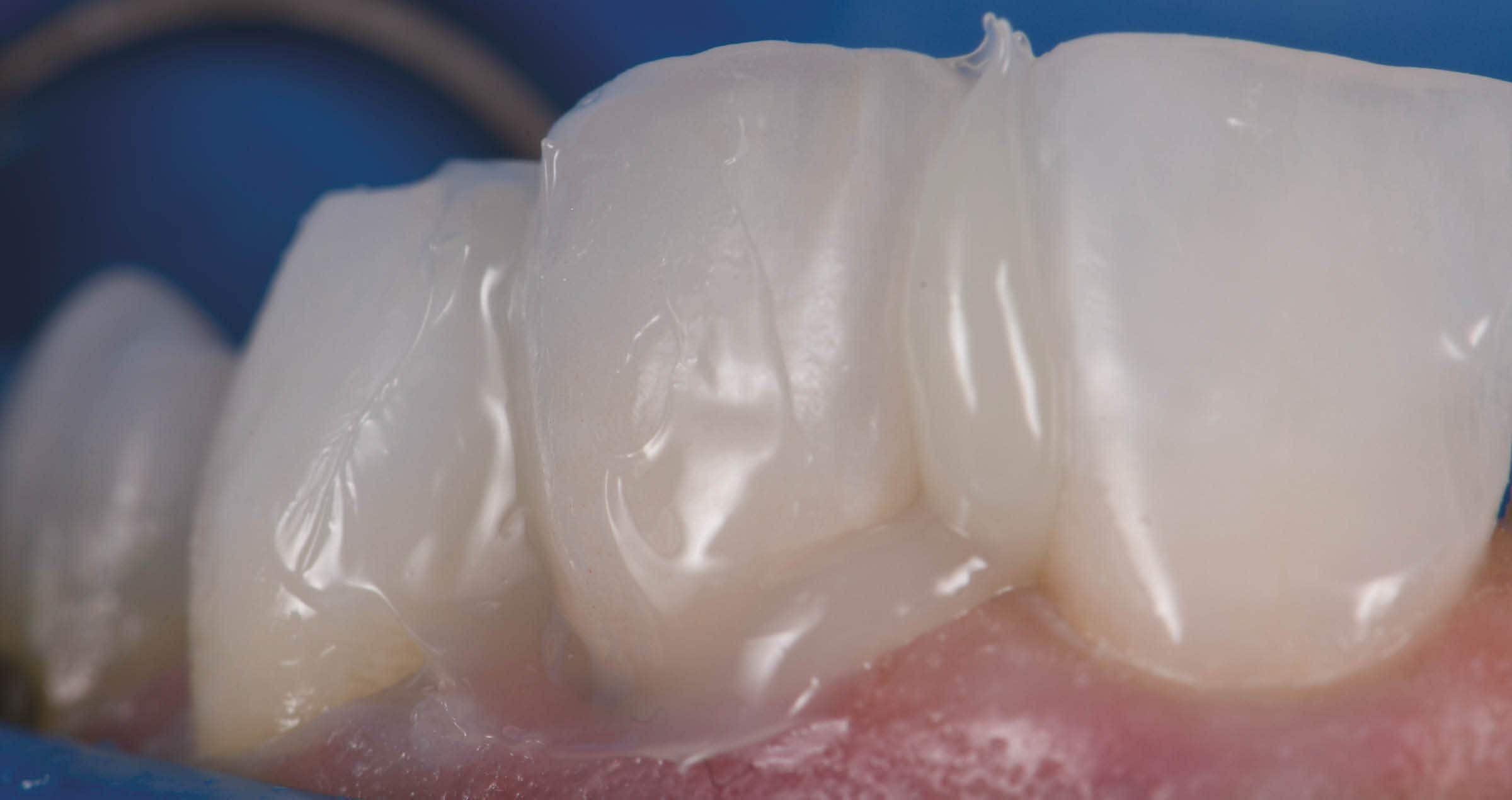
The PANAVIA™ family of products, including PANAVIA™ EX, share the concept of “being a resin cement product that opens new dimensions in dentistry”. PANAVIA™ EX was our first resin cement, and it was conceived as a cement for a new era. It can bond to tooth structure and dental metals very well, thanks to the use of the MDP monomer. This important adhesive monomer is still used today in many of our products. Ever since the launch of PANAVIA™ EX, Kuraray Noritake Dental has continued to take on new challenges and has developed many new products in the growing PANAVIA™ family. These include PANAVIA™ 21, a cement in paste form that has a self-etching primer as an accessory; PANAVIA™ Fluoro Cement, a dual-cure cement paste that releases fluoride; and PANAVIA™ F2.0, which can be used with an LED curing unit. The current portfolio consists of PANAVIA™ V5, which features the substantially improved bonding performance that was achieved after a major review of the basic composition of the series, PANAVIA™ SA Cement Universal, which works as a standalone product without separate primers, and PANAVIA™ Veneer LC, PANAVIA™ family’s latest product. The latter is a light-curing resin cement with the specialized purpose of bonding laminate veneers.
In retrospect, what did the introduction of PANAVIA™ EX mean to Kuraray Noritake Dental?
In the development of new resin cements, it is important to quickly respond to the rapidly changing trends in the market. Whenever new prosthodontic treatment concepts appear – like adhesive bridges as a minimally invasive treatment option replacing a single tooth – or new restorative materials are introduced, such as different types of ceramics – we need to check if our resin cement systems are compatible with the tasks that come with these changes, as well as possibly developing new ones. Following the launch of PANAVIA™ EX, we received a wide range of feedback from experts working at dental clinics and laboratories. We leveraged this feedback in subsequent development projects, always striving to stick close to the clinical setting. After Kuraray Medical Inc. merged with Noritake Dental Supply Co., Limited, this ethos was embedded in the work ethic of all employees of Kuraray Noritake Dental.
| Among the new adhesive monomers being developed, we decided to use the MDP monomer, because it features excellent bonding to tooth structure and metal alloys used in dentistry, as well as superb resistance to water. |
Can you give us a brief history of the PANAVIA™ EX journey to the currently available PANAVIA™ family portfolio?
Since the launch of PANAVIA™ EX 40 years ago, six different PANAVIA™ products have been released. Each of them has received high acclaim for their unique features, both in the Japanese resin cement market and abroad. For 40 years, we have been improving PANAVIA™ in response to the demands of the times. We developed a product with increased adhesion when non-retentive preparation designs (adhesive bridges) and smaller bonding surfaces (due to less invasive preparations) became popular. And for users concerned about secondary caries, we developed a material with fluoride-releasing properties. At the same time, we focused strongly on making dental cementation easier by finding ways to make our resin cements bond well to various types of crown-restoration materials, including precious metals and ceramics. During these drives towards improvement, “achieving reliable general luting” has always been at the forefront of our goals. We believe that the successful evolution of the PANAVIA™ brand owes a great deal to our incessant efforts to obtain a high level of bond strength to dentin after chemical polymerisation”.
How did the R&D department evolve over the years?
Initially, our efforts in the development of dental materials had focused on bonding agents and restorative composite resins. PANAVIA™ EX was just one of our new development projects and only a few staff members were assigned to that product. After PANAVIA™ EX was launched in 1983 and it was accepted worldwide, our product line-up of resin cements was expanded considerably. Consequently, we have increased the number of development staff assigned to resin cements and set up a special development team responsible for the self-adhesive resin cement product line that includes PANAVIA™ SA Cement Universal. As a result, the size of the team assigned to resin cements has expanded substantially.
How did production change?
When PANAVIA™ EX was launched in 1983, the product was manufactured exclusively for the Japanese market in a relatively small facility. Today, in order to produce all products of the PANAVIA™ family for the global market, we have automated our production facilities and increased the production equipment and systems dedicated to producing the resin cement paste. To support our product quality, we have also set up a quality control system that assures we turn out safe and high-quality products, drawing on over 40 years of technical knowhow and experience in the production of resin cements.
For 40 years, we have been improving PANAVIA™ in response to the demands of the times.
When did external researchers start showing interest in PANAVIA™?
The development of PANAVIA™ EX was carried out with the active participation of researchers at a dental college in Japan, involving such activities as performing basic adhesion tests and experimenting with clinical applications using adhesive bridges. At that time, resin cements that provided a strong bond to tooth structure or metal alloys were not widely used. I believe that overseas researchers were interested in the development of PANAVIA™ EX at a relatively early stage, for this reason.
What current concept do you have in mind as you continue developing your adhesive cements?
We have two basic central concepts: “Achieving greater bond strength” and “Delivering easier handling characteristics”. I think that the shades of resin cements are also devised in each product in order to get the most of the characteristics of aesthetic restorative materials. At our company, we have embodied “achieving greater bond strength” in PANAVIA™ V5, and “delivering easier handling characteristics” in PANAVIA™ SA Cement Universal. We will continue to explore the development and introduction of various new technological applications, to bring even higher performance products to market.
What do you think is the strength of Kuraray Noritake Dental’s R&D team?
We conduct R&D activities continuously, focusing on the development of luting materials. In our product development department, the same person is often responsible for one product category over long period of time. For example, I have been engaged in the development of PANAVIA™ products for much of my time with the company. The result is that each person in the development department can be said to be an expert in a certain category of products. They leverage the technical knowledge acquired in the past for the development of new products, resulting in entirely new discoveries.
Do you have any ideas about what the future of PANAVIA™ will be?
We will continue to focus on the development of even simpler, easier-to-use resin cements suitable for a wide range of applications – products based on the concept of universality. This should allow users to focus more on the actual treatment than ever before, while of course delivering a strong and durable bond between the tooth structure and the restoration.
MITSUNOBU KAWASHIMA