Clinical case with CLEARFIL MAJESTY™ ES-2 Universal shades
By Dr Luca Dusi
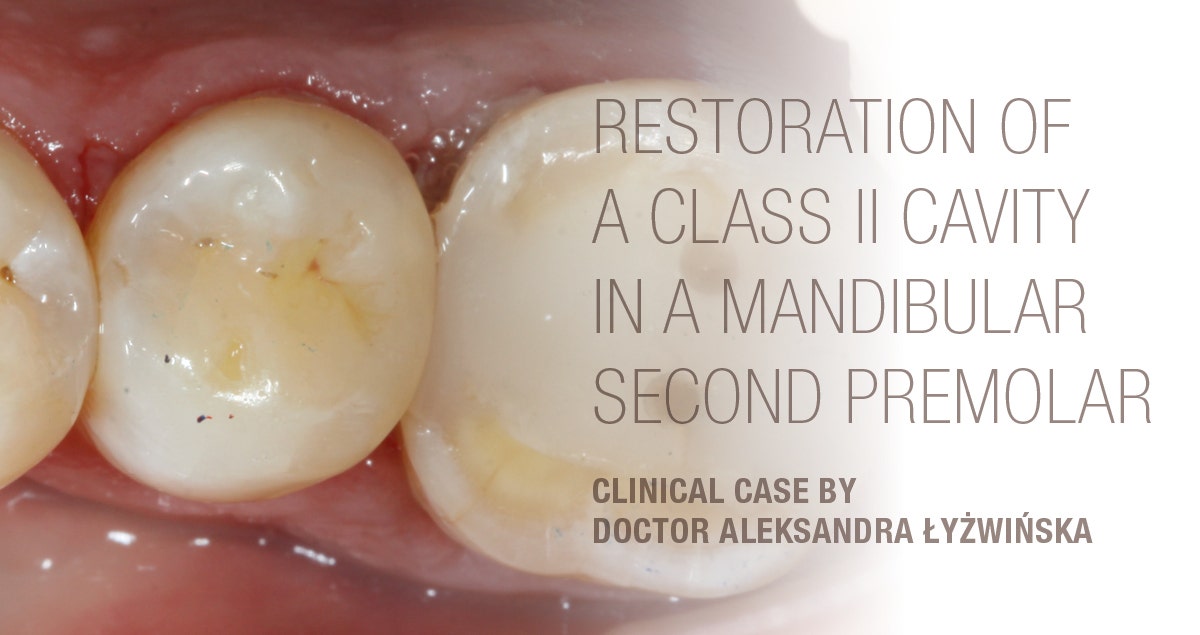
For purely aesthetic reasons, this patient asked for the reconstruction of her cone-shaped upper right lateral incisor (12). The patient was offered a treatment including a first phase of orthodontic therapy aimed at recovering the space necessary to be able to reconstruct the lateral incisor to its ideal size. As the patient refused to undergo this orthodontic therapy, it was decided to restore the tooth with resin composite and match its size to the space already available.
The adhesive system used was CLEARFIL™ SE BOND 2, while the restoration was created with the new composite CLEARFIL MAJESTY™ ES-2 Universal. Although this material is designed for the single-shade technique with only two shades matching the anterior tooth shades, I decided to combine both pastes to achieve the best possible outcome. The shade UD (Universal Dark) was used to reconstruct the cervical and central portion of the lateral incisor. The incisal portion was restored with UL (Universal Light).
Fig. 1. Initial situation with a cone-shaped upper right lateral incisor (12).
Fig. 2. Image of the initial situation taken with a polarising filter for shade evaluation purposes.
Fig. 3. The new CLEARFIL MAJESTY™ ES-2 Universal composite with only two shades for the anterior region was chosen. It offers a good optical integration thanks to Kuraray Noritake Dental’s Light Diffusion Technology.
Fig. 4. Shade determination with the aid of cured samples of CLEARFIL MAJESTY™ ES-2 Universal UL (Universal Light) and UD (Universal Dark) on the tooth surfaces.
Fig. 5. Isolation with rubber dam.
Fig. 6. CLEARFIL™ SE BOND 2 used for the establishment of a strong bond between the tooth structure and the composite material.
FINAL SITUATION
Fig. 7. The universal composite blends in well with the adjacent teeth regarding its colour and surface finish.
Dentist:
- Graduated with honors in Dentistry and Dental Prosthetics at the University of Milan in 2010.
- In 2011/2012 and 2012/2013 he held the position of Adjunct Professor for the teaching of Prosthetic Technologies at the University of Milan-Bicocca.
- Member of SIdp (Italian Society of Periodontology) and AIC (Italian Academy of Conservation).