Clinical case: Full-mouth rehabilitation using multiple types of Zirconia
This case was conducted by Dr Davide Cortellini, owner of Studio Cortellini in Riccione in Italy, and dental technician Angelo Canale, owner of Canale dental laboratory in Rimini in Italy.
This patient came to the clinic to improve her chewing ability and aesthetic level. The physical examination revealed the presence of several endogenous erosive lesions that made chewing difficult, in addition to partly affecting the esthetics due to decrease in enamel thickness and the presence of dyschromic composite restorations. The possibility of using the new types of both tetragonal and cubic multilayer zirconia made it possible for us to plan the complete covering of all the elements with extremely conservative crowns with thicknesses between 0.5 and 1 mm in the axial and occlusal areas and up to 0.2 mm at the margin.
VERTICAL PREPARATIONS
Very conservative vertical preparations were carried out in the enamel without anesthesia. In the upper arch, the front group was prepared for full-veneer crowns, while the lower front group was treated with conventional lithium disilicate veneers without interproximal separation. In this case too, vertical preparations were carried out without finishing line. The impression was made using a 3Shape TRIOS intraoral scanner. The technician modeled the zirconia restorations that were then completed by the ceramist.
Knife Edge Preparation
| No finishing line | |
SCANNING SEQUENCE
| 1. Temporary | 2. Lower arch |
| 3. Upper arch | 4. Bite |
Digital DV models of temporary teeth
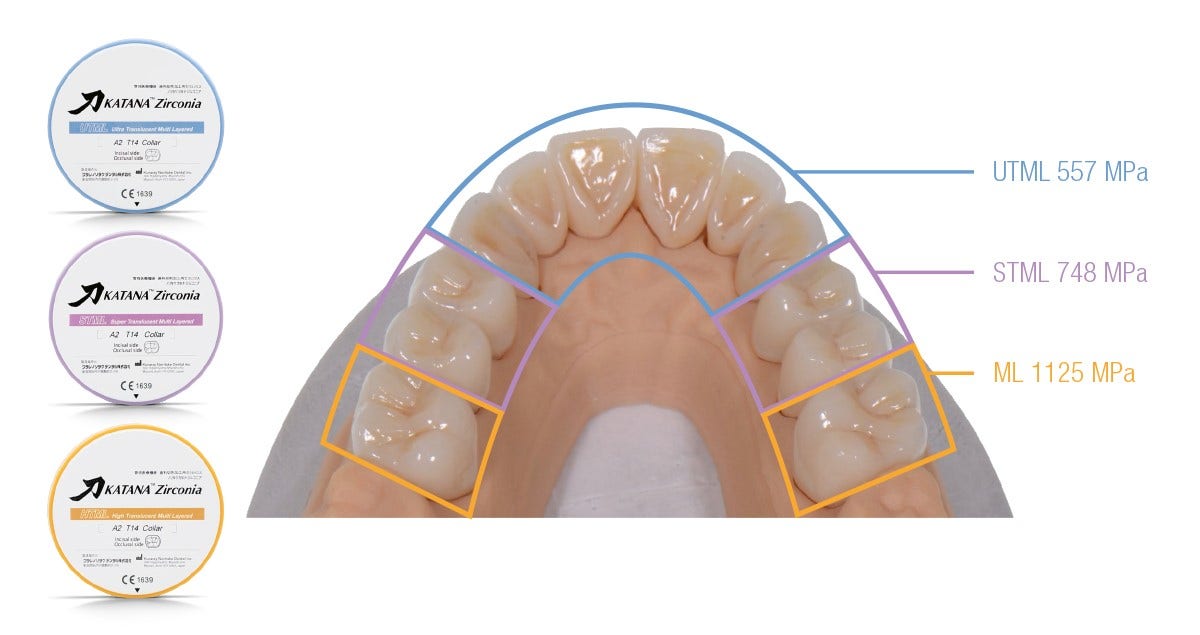
The three different materials were selected on the basis of the specific positions inside the mouth:
- UTML for the anterior teeth
- STML for the premolars
- HTML for the molars
The final result shows excellent integration between the 3 different types of zirconia and a good natural feeling.
| Bucco-lingual thickness: 0.6 mm | Interproximal thickness: 0.5 mm |
MINIMAL PREP KATANA™ (KATANA™ MICRO LAYER)
HARMONIC OPTICAL INTEGRATION
The full-mouth rehabilitation procedure using three different types of zirconia led to a functional and beautiful treatment outcome. The optical integration between the materials is excellent and the high translucency especially in the anterior region creates a true-to-life appearance.
| Initial situation | Final situation |
APPROACH WITH MINIMAL INVASIVE PREPARATIONS - REPORT ON THE SELECTION OF MULTI-LAYERED ZIRCONIA
Dental zirconia is no longer just the opaque framework material introduced two decades ago. Nowadays, it offers the high strength needed for long-span bridges, dentin-like translucency and strength perfect for thin-walled posterior crowns, or enamel-like optical properties for beautiful anterior restorations - depending on its composition and structure. Kuraray Noritake offers three types of dental zirconia - three with a multilayered structure created using patented powder coloring technology. They differ with regard to their optical and mechanical properties, which makes it possible to choose an ideal material for every clinical situation.
Dentists:
DR. DAVIDE CORTELLINI
Dr. Cortellini graduated with honours in Dentistry and Dental Prosthetics from the University of Siena in 1992. He won the scholarship of the Italian Society of Periodontology for the year 1994-95. He then received the opportunity to attend the Department of Periodontology and Fixed Prosthetics of Prof. NP. Lang at the University of Bern in Switzerland, carrying out clinical and research activities. He obtained the title of „Doctor Medicinae Dentium“ (D.M.D.) at the same university in 2000. Dr. Cortellini is the author of scientific publications in international journals of aesthetic dentistry. He is an active member and advisor to the Italian Academy of Prosthetic Dentistry, and a member of the International Academy for Digital Dental Medicine. He holds conferences in Italy and abroad and is dedicated to clinical activity in his own practice in Riccione, where he primarily focuses on aesthetic and digital prosthetics and complex prosthetic rehabilitation.
CDT. ANGELO CANALE
Mr. Canale is a dental technician graduated high school in 1981. He’s the owner of a dental laboratory in Rimini since 1986. He is specialized in fixed prosthesis on natural teeth and on implants with a metal free approach using different kind of materials. He is always interested about digital technique using CAD-CAM systems (in his laboratory the 80% of the work comes from digital impressions). He is co-author of international publications on PPAD, QDT, EJED and THE JOURNAL OF ADHESIVE DENTISTRY concerning the use of metal free in prosthesis. He is a speaker in national and international congress.