Zirconia in dentistry
Zirconia ceramics are increasingly being used for dental prostheses. In the past, they were used as a substructure that was baked with porcelain; nowadays, monolithic zirconia prostheses have been made possible by the introduction of aesthetic zirconia ceramics varieties. They are used more and more, even as RBFDPs (Resin Bonded Fixed Dental Prosthesis).
There is currently quite a lot of discussion about zirconia. So much the better, because it keeps the dynamics of the subject alive. Is it possible to adhesively cement zirconia? Is it permissible to sandblast zirconia? Is it feasible to polish zirconia? Is wear of the antagonist an issue? And so on and so forth.
New dental technologies and materials have been developed in recent years to meet the demand for aesthetic, biocompatible and metal-free prostheses. Although porcelain has been used as an aesthetic dental material for more than hundred years, its restrictions are now well-known. It is the fragility of porcelain (low flexural strength and fracture toughness) in particular which restricts its application in areas where the exertion of massive force on the material is a factor. Zirconia has a high flexural strength and is therefore suitable for multiple dental applications.
Development
The first generation of zirconias used in dentistry belonged to the Partially Stabilised Zirconia (PSZ) class. This type of zirconia, stabilised with yttrium oxide, was composed of a mix of monoclinic, tetragonal and cubic crystals but is no longer used nowadays. The so-called Y-TZP variant was then used for many years, and still is. Its main characteristics are high flexural strength (> 1.000 MPa) and an opaque white appearance. For the most part, this variant is composed of tetragonal crystals of a few hundred nanometers. To keep the material stable at room temperature, approximately 3 mol% of yttrium oxide is added to the composition, which is why it is sometimes referred to as 3Y zirconia.
In order to improve its aesthetic properties, a start was made on the development of a new variety, so-called cubic zirconia. Cubic zirconia is characterised by a high translucence, meaning that a lower flexural strength must be accepted. Admittedly, the flexural strength of this variant is lower than that of the tetragonal variety, but still much higher than the flexural strength of lithium disilicate. It also contains more yttrium oxide; approximately 5 mol%.
Crystal phases
We currently know zirconia crystals in three varieties: monoclinic, tetragonal and cubic. In general, zirconia only exists in the monoclinic phase at room temperature. Monoclinic zirconia has low strength as well as low translucence. Tetragonal zirconia crystals are metastable and can only exist at room temperature after having been stabilised with yttrium oxide, among other metal oxides. The characteristics of tetragonal zirconia are that it is strong, but at the same time devoid of aesthetic
properties. Cubic crystals are stable and ensure improved translucence. Although prostheses made from cubic zirconia are not as strong as the tetragonal variety, they are highly aesthetic, and are even suitable for monolithic restorations in the aesthetic zones.
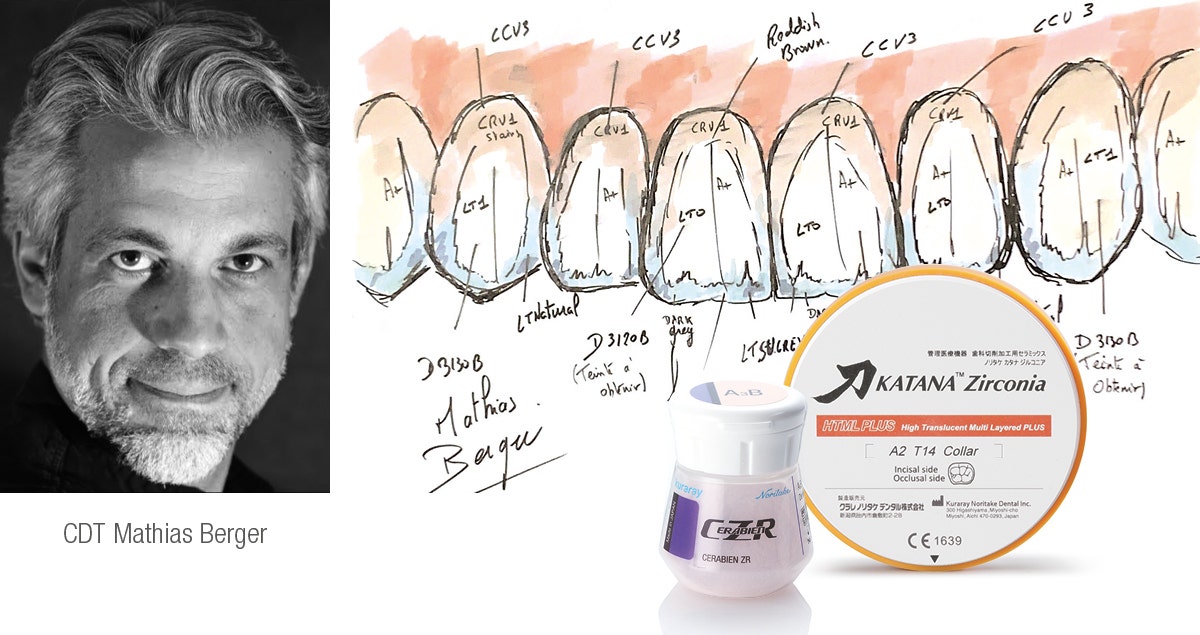
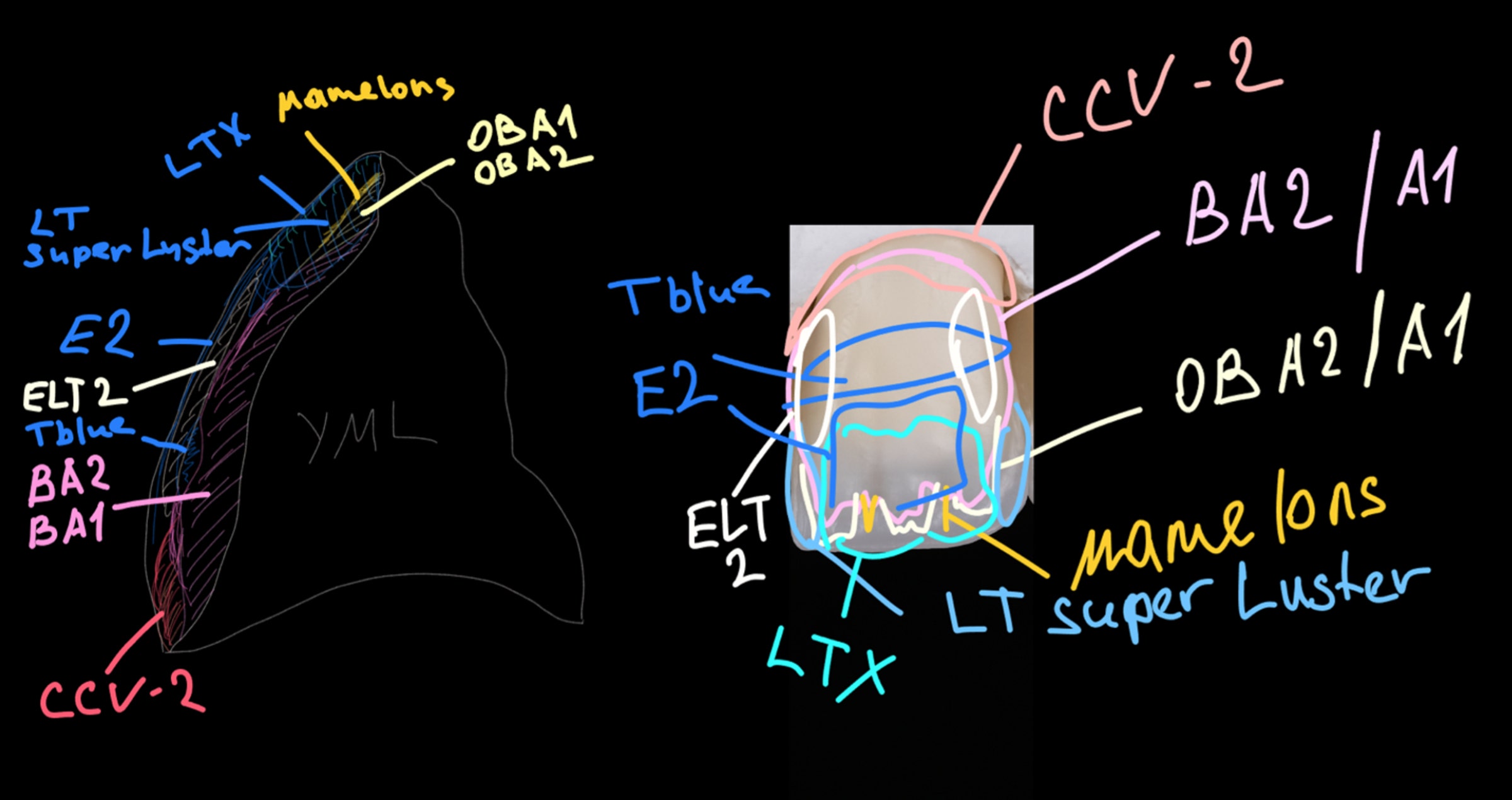
Multilayer
KATANA™ Zirconia ML, STML and UTML, as well as the latest KATANA™ Zirconia Block, are so-called multilayer zirconias. These products are built up of four layers with an ascending degree of translucency, ranging from the more opaque and coloured body layer (cervical), through two transitional layers, to the translucent incisal edge (occlusal/incisal). The invisible transition from one layer to another is achieved using a unique process. The secret is in the specific distribution of particles during the pre-sintered stage (continuous gap grading). In combination with the cold isostatic pressing method, this ensures material of an outstandingly high quality.
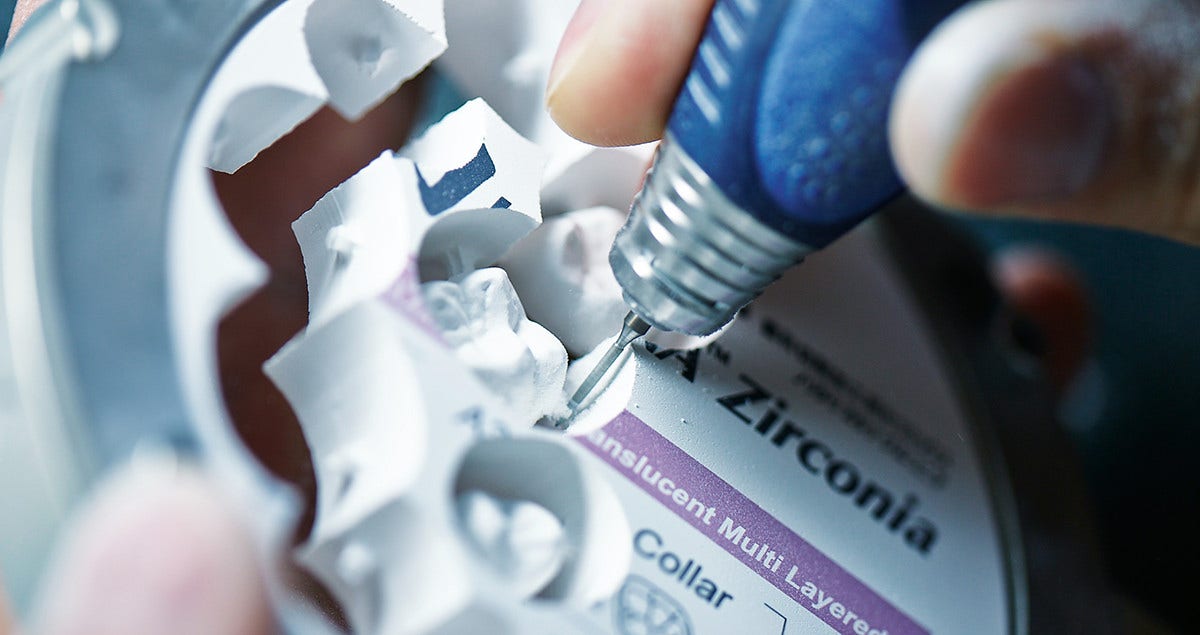
KATANA™ Zirconia Block
The use of KATANA™ Zirconia Block makes it possible to produce a complete monolithic zirconia prosthesis in a short time. This block was developed to be used within the CEREC workflow. After scanning, the prosthesis is ground for approximately 15 minutes and can then be sintered in the SpeedFire oven in just half an hour1). KATANA™ Zirconia Block shares the properties of KATANA™ STML and can be used for the production of single-unit prostheses such as full crowns for both anterior and posterior applications.
Wear of the antagonist
The question of whether zirconia prostheses are harmful to the antagonist would seem to be justified; after all, this is a very hard material. Hardness, however, does not relate directly to the abrasive properties of a material. Smoothly polished zirconia is minimally abrasive, something which has been corroborated by multiple studies2). Glaze, porcelain, lithium disilicate and even enamel are all more abrasive for the antagonist.
CAD/CAM
Thanks to emerging digital solutions (CAD/CAM) combined with the possibility of executing fixed partial dentures (FPDs) in monolithic zirconia, a fully digital workflow - from scan to prosthesis - is now feasible.
Sandblasting
Sandblasting using alumina is the standard method for the roughening of zirconia. In order to reduce the decline from the tetragonal crystal stage to the monoclinic stage, it is recommended that sandblasting be carried out at a maximum pressure of 2.5 bar using 50 micron aluminium oxide particles as a maximum3). In practice, zirconia is also frequently sandblasted tribochemically, for example, by means of CoJet (3M). The results achieved with this method are variable. In the case of limited pressure (2.5 bar as a maximum) there is a risk that the energy will be insufficient to achieve an effective and complete fusion between the silica and the zirconia surface. It is therefore recommended that CLEARFIL™ Ceramic Primer Plus be used for adhesive connection with the sandblasted surface. The silane in this ceramic primer bonds chemically with the silica, while the MDP bonds with the areas of zirconia not covered by silica. The use of silane alone does not provide an adequate basis for a reliable result4). Sandblasting with alumina, however, followed by priming with CLEARFIL™ Ceramic Primer Plus, is a well-proven and reliable method to ensure effective bonding to zirconia5).
Not etchable, but certainly bondable
Zirconia is not – or is barely – etchable with the etching technology available (HF). In addition, it cannot be recommended that zirconia be treated with phosphoric acid, because of the bonding of phosphates to the surface of the zirconia, which will inhibit a chemical activation of the surface for some adhesive cementation systems. The question of whether an etching product should be used is a valid one; after all, chemical etching is not necessary to achieve surface roughness. Achieving surface roughness is, however, a logical option, and roughening by means of sandblasting would seem to be the most appropriate method for zirconia. Thereafter, chemical bonding is ensured using a phosphoric functional monomer, preferably MDP.
Adhesion principles
Three basic factors are required to achieve the effective bonding of different materials. In keeping with the principles of adhesion, these are: surface enlargement (micromechanical retention), chemical activity (adsorption and electrostatic bonding) and a high-energetic surface to guarantee proper adaptation.
Adhesive bonding
The best method of adhesive bonding for zirconia is the use of a composite cement containing MDP. Professor Mathias Kern published an article about bonding to zirconia using MDP as early as 1998. This study showed that sustainable resin bonding to zirconia can only be achieved using a composite cement with a special adhesive monomer. The monomer used was in fact MDP. In the meantime, many studies have been published about bonding to zirconia.
On the one hand, these studies concern bonding with phosphate monomers (MDP); on the other hand, attention has been paid to the modification of the zirconia surface to render it etchable. The simplest and most reliable method is to sandblast the surface at a low pressure using aluminium oxide, followed by priming with an MDP-containing primer6).
PETER SCHOUTEN,
Technical Manager Kuraray Europe Benelux
1) Depending on the method of grinding/milling.
2) Mörmann W.H. et al. Wear characteristics of current aesthetic dental restorative CAD/CAM materials: Two body wear, gloss retention, roughness and Martens hardness. Journal of the mech. Behavior of Biomedical Materials 20 (2013) 113-125, Janyavula S. et al. The wear of polished and glazed zirconia against enamel. J Prosthet Dent 2013; 109;22-29 Stawarczyk B. et al. Comparison of four monolithic zirconia materials with conventional ones: Contrast ratio, grain size, four-point flexural strength and two-body wear. Journal of the mech. Behavior of Biomedical Materials 59 (2016) 128-138 D’Arcangelo C. et al. Wear Evaluation of Prosthetic Materials Opposing Themselves. Oper Dent 2017 antagonistic surface roughness on the wear of human enamel and nanofilled composite resin artificial teeth. J Prosthet dent 2009; 101: 342-349.
3) Attia A. / Kern M. Effect of cleaning methods after reduced-pressure Air Abrasion on Bonding to Zirconia Ceramic J Adhes Dent 2011; 13: 561-567.
4) Pilo R. Effect of tribochemical treatments and silane reactivity on resin bonding to zirconia. Dent Mater (2017).
5) Kern M. Bonding to oxide ceramics - Laboratory testing versus clinical outcomes. Dent Mater (2014).
6) M. Kern et al., Bonding to zirconia ceramic: adhesion methods and their durability. Dent Mater 14: 64-71, Jan.1998.